Devoted to Memory
Devoted to Memory
Photo by Natalie Yahr
Wisconsinites mobilize to fight Alzheimer's disease
“Do not ask me to remember…”
That’s the beginning of a poem that lives in a frame on the wall of Carolyn Scheuerell’s room at Park Place Assisted Living.
“Just remember that I need you / That the best of me is gone / Please don’t fail to stand beside me / Love me ’til my life is done.”
Kent Scheuerell does just that for his wife, who has been living with Alzheimer’s disease for the past 10 years. Until last December, Scheuerell was his wife’s primary caregiver before circumstances forced her to move into Park Place Memory Care in Platteville, a city in southwestern Wisconsin. He now visits every day.
On some days, they dance together — something they’ve been doing for almost 50 years. “I met her when I asked her to dance,” Scheuerell says, remembering the night when he first led his future wife onto the dance floor.

Kent and Carolyn Scheuerell dance in the lobby of Park Place Assisted Living. (Photo by Natalie Yahr)
Now, they dance in her room to “Smile” by Nat King Cole and Glenn Miller’s “In The Mood.” But today, there will be live music in Park Place’s lobby. Residents will gather around a gleaming baby-grand piano to listen to music, tap their feet, and watch Kent and Carolyn dance. When they dance, he gets his wife back. “When the music starts, she starts swinging and dancing, and smiles more than otherwise,” Scheuerell says.
There is something about being close to a person with Alzheimer’s disease that inspires people to dedicate their energy and resources to fight against it. Scheuerell, who in the beginning was afraid and tried to hide his wife’s diagnosis, now finds himself fully engaged in the larger Alzheimer’s community. Many people across Wisconsin — from individuals to nonprofits and government agencies to university researchers, patients and their caregivers — point to personal experiences with Alzheimer’s and dementia as an inspiration for their involvement. This community is guiding Wisconsin toward a future where caregivers feel more supported, and maybe, thanks to research at UW-Madison, loved ones of those with Alzheimer’s can start hoping for a cure.
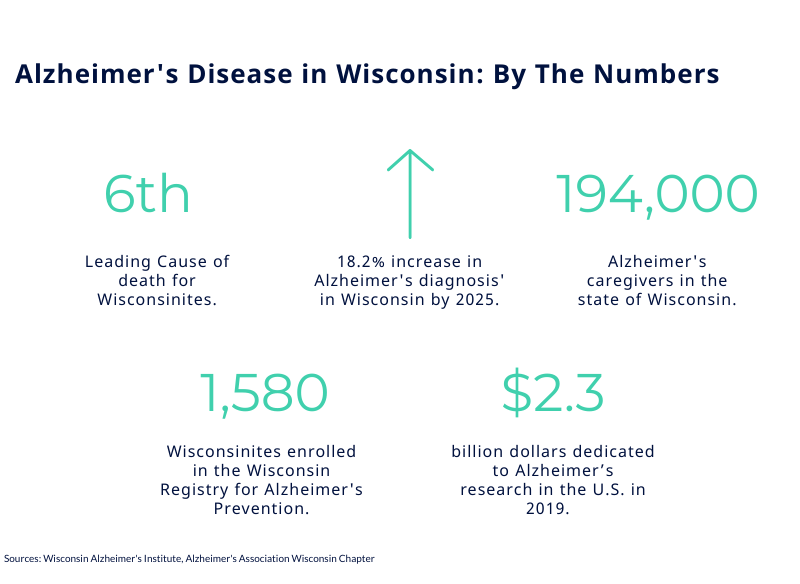
In Wisconsin, loving someone with Alzheimer’s is a common experience. Alzheimer’s disease is the sixth-leading cause of death in Wisconsin, and, according to the Alzheimer’s Association, the number of people 65 or older with Alzheimer’s disease in the state is estimated to increase 18 percent by 2025.
It’s that experience that galvanizes those who are working to beat it. Dr. Nathaniel Chin was finishing his internal medicine residency in San Diego when he got the news that his father had been diagnosed with Alzheimer’s disease. Chin’s father had been a family care physician in Watertown, Wisconsin, a city about halfway between Madison and Milwaukee, and was his son’s inspiration for entering the medical field. His father’s diagnosis further inspired him to enter geriatrics. Chin, 35, is now a memory care provider with UW Health and a researcher with the Wisconsin Alzheimer’s Disease Research Center, where he and his colleagues are trailblazers in Alzheimer’s research.
Shortly after starting a new position as a dementia outreach specialist at the Alzheimer’s and Dementia Alliance of Wisconsin, Becky DeBuhr started noticing some changes in her mother-in-law. “She would have some paranoid thoughts about people stealing her money or taking her purse. She was often misplacing things to the point of not remembering at all where she could find [them],” DeBuhr says. “She explained to us that she felt like she was going to get lost.” Eight years after being diagnosed with Alzheimer’s disease at a local memory diagnostic clinic, DeBuhr’s mother-in-law passed away. DeBuhr now serves as the program director at the alliance, a nonprofit that provides free resources and support to families dealing with Alzheimer’s.
Wisconsin State Rep. Mike Rohrkaste’s mother was in Ohio when she began experiencing dementia. Rohrkaste could not be there to help her every day, but he still had important decisions to make. “Eventually, I had to put my mom in a nursing home because she just couldn’t live on her own. It was too dangerous for her or for others,” he says. “It was unfortunate that I had to do that, because I think that, you know … she might have lived longer if she would have been able to stay at home.” After he leaves office late next year, Rohrkaste will continue in his position as the executive director of the Fox Valley Memory Project.
Understanding Alzheimer’s
Alzheimer’s and dementia are not one and the same. According to the Alzheimer’s Association, dementia is a range of conditions defined by loss of memory, language, problem-solving and other skills that make it difficult for those affected to independently manage their lives. Alzheimer’s disease is an abnormal process in the brain that causes symptoms such as cognitive impairment or dementia. But having dementia does not necessarily mean that a person has Alzheimer’s, just as Alzheimer’s disease could cause mild cognitive impairment but not dementia.
Symptoms of Alzheimer’s can manifest in different ways. Scheuerell, 72, knew his wife, also 72, was having trouble when he opened their checkbook one day to find it an unbalanced mess. Carolyn, who had been a bank teller before retirement, always balanced their checkbook perfectly, down to the last penny. When he asked her about it, she seemed not to care.
He went with her to the next doctor’s appointment, where it became clear that his wife was not as mentally fit as before. Scheuerell remembers asking the doctor, “Where do I go?” and that’s when he was introduced to the local Aging and Disability Resource Center and the Alzheimer’s and Dementia Alliance. Those organizations saved him, Scheuerell says.
A network of support
From the beginning of a journey with Alzheimer’s and dementia to the end, Wisconsin patients and caregivers alike have the support of public and private organizations. Wisconsin does this uniquely well, according to DeBuhr.
Spread across the state, Wisconsin’s Aging and Disability Resource Centers and the Wisconsin Alzheimer’s Institute’s affiliated Dementia Diagnostic Clinic Network bring quality information, dementia expertise, medical screenings and outreach specialists to local communities, especially in rural areas.
“That’s really the progressive part here in Wisconsin — that no matter where you are in the state, most people can pretty much get to a local memory diagnostics clinic,” DeBuhr says.
Through these networks, the centers’ dementia care specialists and the alliance’s dementia outreach specialists connect with people in counties across Wisconsin. They have the initial difficult conversations, which are the catalyst for connecting patients and caregivers, like Scheuerell, to other resources in their local communities.
The more connected a person becomes, the more aware they are of the resources that are available to them such as free classes, support groups, financial advice and more. Scheuerell has taken nearly 20 of the alliance’s free classes, including one on preparing for the end.
He also attends one of the alliance’s support groups with people who have become like family. These groups provide a space where caregivers can ask difficult questions and receive honest answers that only other caregivers can give. Everyone breaks down the first time they visit the support group, Scheuerell says, but the bond they create is special.
“When you‘re telling each other these things you really do bond with those people, you‘ve got something special,” he says.
The alliance also offers memory cafes, where caregivers can take their patients to “experience music and art and movement, connection and cognitive stimulation,” DeBuhr says, “and we do a lot of laughing.” Twice a month, Scheuerell and his wife go to one of these memory cafes. Sometimes, Scheuerell breaks out his Elvis impersonation for these gatherings.
When asked how he feels at these memory cafes, Scheuerell breaks down. “If my wife smiles, it’s worth it,” he says. “If she’s having a good day, I am, too.”
Never in his wildest dreams did Scheuerell imagine that he would be so involved in the Alzheimer’s community. But by default, he has become a liaison between the help and those who need it. Now, he always carries a card in his wallet that outlines who to contact at the alliance.
“In the beginning, it’s so hard to talk about things like that,” Scheuerell says. “But people helped me by telling me things like that, so I say, well, now it’s my turn to help them.”
An uncertain future
It is difficult for families of Alzheimer’s and dementia patients to know what each day will bring. Scheuerell says it can be difficult to plan for the future, including navigating financial needs and understanding the legal intricacies of their situation.
When caregivers face more and more responsibility, planning for the future can get lost in the everyday challenges of caring for a loved one with Alzheimer’s or dementia.
“We don’t know what’s going to happen,” Scheuerell says, “so we just have to do what you have to do.”
As a member of the Wisconsin State Dementia Plan Steering Committee, which helped produce the Wisconsin Department of Health Services’ new Dementia Plan for 2019 to 2023, Rohrkaste understands the importance of supporting caregivers.
 “The help can vary between health care help, to potential nursing home options, to just staying active in the community, or getting personal care workers to come in or getting respite care,” he says. “Respite care is important for the caregivers … [if] they don’t take care of themselves, then their health risks go way up.”
“The help can vary between health care help, to potential nursing home options, to just staying active in the community, or getting personal care workers to come in or getting respite care,” he says. “Respite care is important for the caregivers … [if] they don’t take care of themselves, then their health risks go way up.”
But it’s not just legislators and nonprofits that can contribute to this community. Through the Wisconsin Registry for Alzheimer’s Prevention, people across Wisconsin can participate in the university’s groundbreaking research. The registry is a home-grown program, accepting only participants who have lived in Wisconsin. The study has been running since 2001, when it was created by Dr. Mark Sager, the same physician who diagnosed Chin’s father with Alzheimer’s.
The registry is incredibly important for building a long-term database for understanding potential causes of, or predispositions to, Alzheimer’s disease.
“It is one of the most important and foundational studies in the entire world,” Chin says. “[It] is probably the first of its kind to recruit people who had a family history of Alzheimer’s disease and not just the person who has Alzheimer’s disease.”
As the medical director of the study, Chin recognizes that there is an environment in Wisconsin that makes the research possible. The registry study is an example of the Wisconsin Idea: people throughout the entire state are invested in solving the question of Alzheimer’s and dementia.
“I think there’s a real relationship between the research that we’re doing and the researchers, and the community that’s engaging in that research,” Chin says. “And I do think that that is something very special.”
Researchers are also seeing a big increase in funding, making it an exciting time for the field, according to Chin. The National Institutes of Health will spend more than $2 billion on Alzheimer’s disease research in 2019 and are expected to commit $350 million more in 2020. For Chin, this means an acceleration in the pace of research.
“I think we’re at this precipice where something is going to happen in the next few years that is going to be monumental for the field,” he says. “I do think 2020 marks a change in the acceleration towards that big moment when we actually have something very meaningful to share with people who have Alzheimer’s.”

The Scheuerells have been married for nearly 50 years. (Photo by Natalie Yahr)
While researchers continue to work toward a breakthrough, the community will continue offering creative solutions to better the quality of life for patients and caregivers.
“For now, the Alzheimer’s Alliance will stay steady in our support of families,” DeBuhr says.
But, she adds, the most important factor for those investing their time, energy and resources is keeping hope in mind.
“I think that looking into the future, probably for a caregiver and the person with dementia, is to always keep the idea of hope central,” DeBuhr says. “That today may not be a great day, but there are things that we can try, or we can learn, or we can do, to always keep hope as part of the journey with dementia.”
Scheuerell knows that a cure would come too late for his wife, but he takes comfort in knowing that it may give their children peace of mind.
And without every resource that helped them along the way, they could not be here in the lobby of Park Place, waltzing to delicate piano music. And you can almost picture them as they were, nearly 50 years ago, when he first asked her to dance.
Hear from Scheuerell...

Maddie Boulanger | Lead Writer
Senior studying strategic communication with a certificate in digital studies